Dr Harshada Rajadhyaksha

In Sanskrit, the word “Prakruti” means “Nature”: the primal motive force of the Universe; Ayurveda recognized that no two humans are alike, and called this basic, very unique, individual constitution, “Prakruti”.
At Prakruti Sports Science and Physiotherapy Clinic, we provide the environment, expertise, and support required to assist natural healing.
True healing begins from within the self: Doctors and Healers can only assist along the process. After 22 years, we continue to remain humble in our approach to diagnosis and treatment, our focus remains on the complete wellbeing of our patients, and we continue to promote the prevention of lifestyle-related diseases in the community.
Our patients’ trust and faith in us, and our honest concern for their wellbeing has been the foundation of our success.
Diabetes Mellitus
Our body is made up of numerous cells and they are working round the clock throughout life. Food is their fuel, and the way our body handles the food that we eat is the determinant of how our cells work. When the energy delivery mechanism fails cellular function is affected, and things begin to go wrong. Diabetes is thus at the center of several illnesses.
But our body has a tremendous capacity to heal itself, and our job is only to keep it in an environment where it can do so. Please do read an article written by Dr. Devendra Raut for World Diabetes Day.
- Dr. Harshada Rajadhyaksha
Diabetes in India:
According to Diabetes Atlas 4th edition published by the International Diabetes Federation, the number of people with diabetes in India around 50.8 million in 2010 is expected to rise to 69.9 million by 2025 unless urgent preventive steps are taken.
Origin of Diabetes Mellitus:
Diabetes has been known since the first century B.C.E., when a Greek physician, Aretus the Cappadocian, named it diabainein, meaning “a siphon,” referring to excessive urination. The word diabetes was first recorded in 1425, and in 1675, the Greek mellitus, “like honey,” was added, to reflect the sweet smell and taste of patient’s urine.
Diabetes Mellitus:
Diabetes mellitus is a group of metabolic diseases in which a person has high blood sugar, either because the body does not produce enough insulin, or cells do not respond to insulin that is produced.
Types of Diabetes Mellitus:
- Type 1 diabetes (Absolute insulin deficiency).
- Immune-mediated diabetes: Accounts for only 5–10% of those with diabetes, also known as insulin dependent diabetes or juvenile-onset diabetes, results from a cellular-mediated autoimmune destruction of the B-cells of the pancreas.
- Idiopathic diabetes: No known aetiologies. This form of diabetes is strongly inherited, lacks immunological evidence for B-cell autoimmunity and is not HLA associated.
- Type 2 diabetes (ranging from insulin resistance with relative insulin deficiency to an insulin secretory defect with insulin deficiency): Accounts for 90–95% of those with diabetes, also known as non–insulin-dependent diabetes or adult onset diabetes, encompasses individuals who have insulin resistance / insulin deficiency.
- Gestational Diabetes Mellitus: Occurs when women without previous history of diabetes develop high blood glucose level during her pregnancy.
Symptoms of DM:
High blood sugar patients show classical symptoms of polyuria (frequent urination), polydipsia (increased thirst), polyphagia (increased hunger), at times weight loss and blurred vision.
Diagnosis of DM:
(Prediabetes level)
- Fasting Plasma Glucose (100 – 126 mg/dl)
- 2 h Oral Glucose Tolerance test (140 – 199 mg/dl)
- HbA1C range of 5.7–6.4% (HgA1C reflects time averaged blood glucose during the previous 2 and 3 months).
Note: Levels exceeding the upper limit is considered as diabetic
Complications:
Retinopathy (potential loss of vision)
Neuropathy (risk of foot ulcers and amputations)
Nephropathy (leading to renal failure)
Cardiovascular complications
Ulceration
Micro-vascular complications and macro-vascular disease like coronary artery, cerebro-vascular and peripheral vascular diseases
Lifestyle, Genetics, and Medical Conditions:
Type 2 DM is primarily due to lifestyle factors and genetics. A number of lifestyle factors like physical inactivity, sedentary lifestyle, cigarette smoking and generous consumption of alcohol contribute to development of type 2 DM. Obesity has been found in approximately 55% of type 2 DM patients.
Management:
Insulin replacement therapy is mainstay for type 1 DM patients; while diet and lifestyle modifications are considered the cornerstone for management of type 2 DM. Oral hypoglycaemic agents are also useful for type 2 DM patients. Eating high fibre and unsaturated fat and diet low in saturated and trans-fats and glycemic index, regular exercise, abstinence from smoking and moderate consumption of alcohol should be implemented as part of lifestyle modification.
Exercise:
- Aerobi exercise (walking briskly, swimming, dancing, riding bicycle or playing sport)
- Strength training to build muscle (do strength training with hand weights, elastic bands or weight machines 2-3 times/week)
- Stretching exercises or yoga (Stretching increase flexibility, lower your stress and help prevent sore muscles)
- Extra activity to daily routine (Gardening, walk when you talk)
Talk to healthcare professional before you start planning your exercise routine
Herbal treatment of diabetes:
In last few decades eco-friendly, bio-friendly, cost effective and relatively safe, plant-based medicines have been the main stream. World Health Organisation (WHO) has listed 21,000 plants, among these 2500 species are in India, out of which 150 species are used commercially on fairly large scale for medicinal purposes around the world. India is the largest producer of medicinal herbs and is called the botanical garden of the world.
A list of medicinal plants with proven anti-diabetic and related beneficial effects and of herbal drugs used in treatment of diabetes like Banaba leaves, Indian Gooseberry (amla), Cinnamon, Okra, Curry leaves etc.
Diet:
Eat more of:
- Healthy fats from raw nuts, olive oil, fish oils, flax seeds or avocados
- Fruits and vegetables – ideally fresh, the more colourful the better; whole fruit rather than juices
- High-fiber cereals and breads
- Fish and shellfish, free-range chicken or turkey
- High-quality protein such as cheese, unsweetened yogurt etc.
Eat less of:
- Trans fats from deep-fried foods
- Packaged and fast foods, especially those high in sugar, baked goods, sweets, chips, desserts
- White bread, sugary cereals, refined pastas
- Processed meat and red meat from animals fed with antibiotics and growth hormones
- Low-fat products that have replaced fat with added sugar i.e. fat-free yogurt
- Dr. Devendra Raut
Be stronger than the challenge, and let the challenge make you stronger!!!
Be stronger than the challenge,
And let the challenge make you stronger!
Our young therapist Dr. Priyanka Bodhe has written a wonderful article inspired by a woman she knows. Read what she has to say about dealing with one of the outcomes of breast cancer treatment, lymphedema.
- Dr. Harshada Rajadhyaksha
Recently, I came across a lady, otherwise healthy, who discovered a pea sized lump in her axilla. Having lost a very dear family member to breast cancer not more than a year ago, she became very conscious and immediately met a doctor to seek medical help. A few tests and they detected her with early stage of breast cancer which has also affected few lymph nodes in the axilla. Within a week she underwent Lumpectomy (surgical removal of the lump). For further management she has been advised few chemotherapy sessions and one radiation.
They say “The best protection is early detection”. But this has also arose few questions in my mind.
- Is breast cancer genetic and only women with family history carry the risk of developing the disease? If it was not for this 37 year old young lady, to have lost a near one to the disease, would she have become aware and alert about the monster that was about to grow in her body so early?
- And will chemotherapy and radiation end her fight or will they leave behind them some scars?
I m not an expert in the topic but witnessing the growing incidence of breast cancer in the community, I would like to highlight certain after effects of cancer treatment and what we as Physiotherapists can do to improve the Quality of life of those affected.
Firstly, let me start by wiping out the belief that family history is the biggest risk factor. Because in reality only 5-10% of cases are due to faulty genes. Thus, regular mammograms and clinical breast examination annually for all women above 40 years of age and every 3 years for women between 25- 40 years of age can help detect the disease in its earliest stage.
Secondly, chemotherapy and radiation therapy might not end her fight as they carry certain side effects such as:
- General de-conditioning and weakness of muscles
- Cancer related fatigue
- Breathlessness
- Joint pain and stiffness
- Soft tissue fibrosis
- Radiation related shoulder capsular thickening
- Lymph edema
- Postural changes
In other patients surgery might be opted for. Surgical management may include a lumpectomy as mentioned earlier or mastectomy-radical or modified.
Post surgery complications:
- Scars and skin adhesions
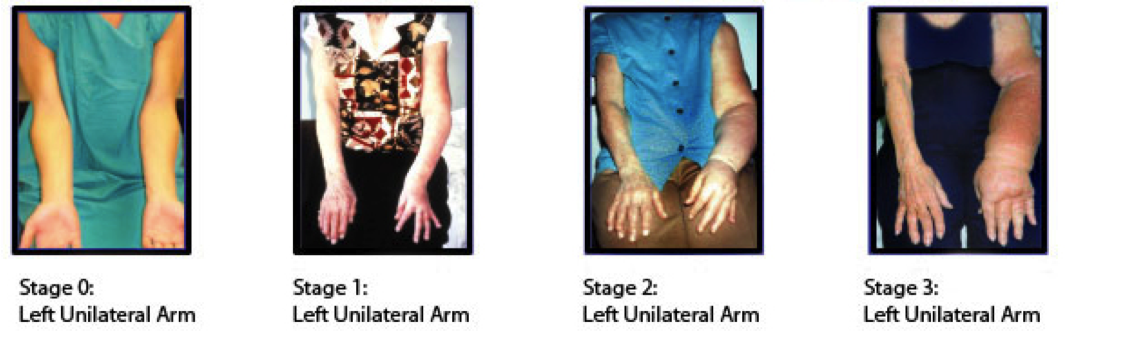
- Swelling/Lymph edema
- Upper limb, trunk and abdominal weakness
- Chest , neck and shoulder muscle tightness
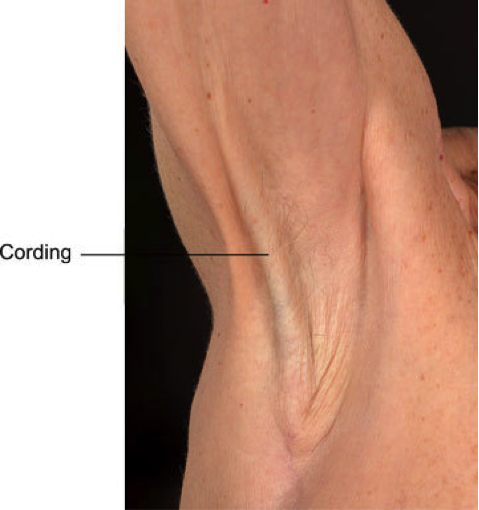
- Axillary web syndrome/ cording with reduced flexibility, pain and weakness of upper limb
How can physiotherapy benefit in preventing and managing these side effects? When should one start physiotherapy?
- Physical therapy integrated with these cancer treatments create a more comprehensive approach to survivorship.
- It reduces mortality by 40% in breast cancer patients
- Among all the known complications, recognition and prevention of lymph edema, is critical in breast cancer rehabilitation.
- Lymphedema manifests itself as swelling in the affected arm because of a blockage of lymph passages and the body’s inability to drain fluid from surrounding tissues.
Treatment for lymphedema includes:
- Education about skin care
- Compression: compression bandages or compression sleeves and garments are designed to create pressure in arm and hand to keep lymph moving in the right direction.
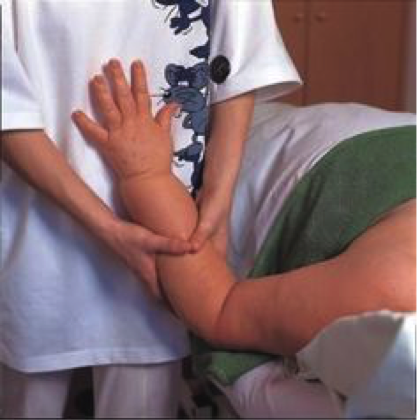
- Manual lymphatic drainage or massage: uses light touch to move excess lymph and fluid out of the tissues and back into the lymphatic vessels.
- Exercise: includes basic mobility and strength exercises, individually designed for every patients by a physiotherapist.
- Hydrotherapy: water offers buoyancy and upthrust. “Water supports us, assists movement and causes resistance leading to strengthening”. Exercising in water will help in improving cardiovascular endurance, reducing lymph edema, improving range of motion and decreasing stress.
Physiotherapy might not be “The answer” to all the complications but it plays a major role and goes a long way in preventing and managing the breast cancer treatment after effects thus improving the quality of life of those who seek help.
Kill cancer, before it kills you…!!!
Turn a setback, into a comeback…!!!
-Dr. Priyanka Bodhe
“You can’t help getting older, but you don’t have to get old.”
“You can’t help getting older, but you don’t have to get old.” _ George Burns
Aren’t we all always looking for tips to stay and look young? The market is flooded with beauty products to achieve this result; the media is overflowing with information to stay “fit”; and billions are spent on cosmetic surgeries to pull off what make up and exercise cannot.
The body is a continuously evolving system, and everyday billions of cells die, another billion new ones taking up their space. As we grow older, this process goes on, but there are lesser new cells generated, and this is inevitable.
Bone being a living tissue, also ages and weakens as we grow older. This is inescapable, but osteoporosis (brittle bones) is preventable!
In our quest to stay young, let us not forget the primary scaffolding of our body that upholds all else!
-Dr. Harshada Rajadhyaksha
Osteoporosis is a “silent disease”, as it progresses without any symptoms until fracture occurs. Your wrist, hip and spine are the common sites for osteoporotic fractures. Post spine and hip fracture, immobilization being essential for healing, still has a detrimental effect on health and quality of living.
Bone is a highly dynamic organ. It constantly undergoes resorption and regeneration. By third decade of life, bone attains its peak mass. As age progresses, in both men and women, balance between resorption and regeneration becomes progressively negative. Post menopause, there is an abrupt drop of oestrogen. Oestrogen hormone plays a crucial role in bone modulation. Thus, we can see old age and oestrogen deficiency are the most critical factors for developing osteoporosis. Besides this, risk factors affecting bone density include genetics (Europeans, Asians), lifestyle (smoking, alcohol, low vitamin D levels due to less sunlight exposure, calcium deficient diet), low physical activity and certain medications.
Confirmatory tests include Bone Mass Density (BMD) analysis which determines both osteoporosis and its early signal osteopenia.
Osteoporosis has no cure but yes we can definitely stop /slow down its progress. Early detection is the best prevention. There are injections available for people who are highly osteoporotic, probably due to any medical condition like prostate / breast cancer, even may be due to prolonged immobilization as that itself causes disuse osteoporosis. These injections needs to be taken on yearly basis to improve bone density as in these scenarios prevention of associated complications is the primary concern.
For elderly population, due to improper muscle strength, balance, coordination there is increased fall risk. Even minimal stress during a fall has a good potential to cause fracture in osteoporotic bones. Simple steps like railings in bathrooms, rooms, maintaining adequate space and good footwear will help reducing the fall risk, thus preventing any incidence of fracture.
One should start working towards modifiable risk factors such as lifestyle modifications. This may include smoking cessation, avoidance of excessive alcohol. In terms of nutrition, one should have calcium and Vitamin D rich foods but also adequate calorie intake to prevent malnutrition. Prevention can be started from any age as goals differ for age groups. For childhood and adolescence – achievement of peak bone mass, middle age – preservation of bone and muscle strength and mass, old age –optimization of gait and balance, muscle strength.
Exercise plays a key role in building and maintaining bone health. Research has proved resistance, aerobic, high impact training, whether done in isolation or combination can improve bone density in osteoporotic persons. One should not rush into unaccustomed exercises (swimming, cycling may be good for your heart but not appropriate to improve bone density). It is important to do what is the most appropriate.
Everything in moderation is always better. Combination of healthy lifestyle, proper nutrition and appropriate goal oriented exercise can prove to be extremely beneficial. No two osteoporotic individuals are same and hence one can always look out for an expert advice for an individualized program.
- Dr. V. Sivajanani
“Love your bones, Protect your future.”
The World Osteoporosis Day has a theme this year of: “Love your bones, Protect your future”, urging people to take early action to protect their bone and muscle health.
Calcium is crucial to bone health, and most of us do not get enough of this mineral in our early life, when it matters the most.
The daily requirement of Calcium in adult life is about 1000 – 1300 mg/ day. It is extremely difficult to reach this figure unless you know how to combine foods.
This is how much Calcium you can get from common foods:
- Try having 1 cup low fat milk/ Soy milk with your breakfast in the morning: Maybe as a smoothie/ with oats/ cereal/ just plain, or with a nutritional supplement. Depending on what you add, you will get about 200 – 300 mg. of Calcium already.
- Have 1 cup Yoghurt (Low fat/ homemade) some time through the day: Maybe with lunch, or with fruit as an evening snack. You will get about 250 mg. of calcium here.
- Try this juice whenever convenient. Please remember to have it as soon as it is made. 1 cup any vegetable (choose watery vegetables like Cucumber, tomato), and others like carrots, beets, sweet potato + ½ cup coriander and mint leaves + 1 stick Celery + 1/2 cup a green vegetable like Spinach or Lettuce + 1 cup fruit (orange is best, but any other like apple, pineapple, etc. will do). Add ½ cup water and all diced ingredients to a mixer and blend well. Serve immediately by straining through a medium sieve, over 2 cubes of ice, and add juice of 1 lemon while serving. Have a large glass, it is refreshing, tasty, and gives you about 150 – 180 mg of Calcium, along with many other minerals equally important to bones (by the way, milk which is such a good source of Calcium, is a poor source of other important minerals)
- The bread, chapatti, idli, dosa, khakra, and other carbohydrates that you eat through the day will give you about 10 mg. Calcium each.
- The dals, lentils, and beans that you eat (white beans are higher in calcium, and soy beans are packed with calcium) will give you another 20-40 mg. of Calcium per cooked ½ cup.
- If you eat nuts, seeds (make sure there is 1 tbsp. sesame seeds), and dry fruits (about 1/3rd cup), this will give you another 80 mg. of Calcium.
- Maybe you will also eat a slice of Cheese (1 slice is 200 mg), or Paneer (50 mg. in ½ cup), or Tofu (200 mg in ½ cup), or an Egg (25 mg), or some Chicken (21 mg. in about a cup), Fish (15 mg in a cup), Quinoa in salad (60 mg in a cooked cup), or other Vegetables (30-40 mg. per cup), or maybe an Ice-cream (85 mg in 1/2 cup serving), or other Dessert (15-100 mg. in ½ cup) through the day.
Here is a sample diet that will give you about 1030 – 1440 mg. Calcium per day, with just about 1500 – 1600 Kcal Energy intake.
Of course you might not eat with this much discipline every day. But if you remember how important calcium is, and how to combine foods, you might always make sure of getting enough.
Sample Menu
|
Breakfast |
1 slice toast
+ 1 slice cheese or ½ cup scrambled tofu OR 1 egg + 1 cup milk |
250 – 400 mg. Calcium |
| Mid – Morning Snack | 1 fruit | 10 mg Calcium |
|
Lunch |
1 chapatti
+ ½ cup dal/ white beans/ chicken/ fish + ½ cup vegetable + 1 cup salad (use 2 florets of Broccoli) + 1 cup low fat yogurt |
350 -450 mg. Calcium |
|
Evening Snack |
1 glass Homemade Vegetable juice OR 1 cup yogurt with fruit OR 1 soy milk with 1 banana OR 1/3rd cup seeds and nuts | 100- 180 mg. Calcium |
|
Dinner |
1 chapatti
+ ½ cup dal/ white beans/ chicken/ fish + ½ cup any vegetable + 1 cup salad OR Green vegetable OR Bhindi |
320-400 mg. Calcium |
Remember not to eat more than 500 mg. of calcium at a time.
Do not exceed 1500 mg. Calcium in a day.
Eat varied sources so that you get all nutrients.
Eat moderate amount of salt and protein. Excess of both will cause loss of calcium.
Do not follow this plan if you have kidney stones/ any other reason to avoid a high calcium plan.
Do take an expert opinion if you do not have an idea about your exact nutritional requirements.
Love your Bones and Protect your Future: Remember, the time to save is now!
Breast Cancer
Breast Cancer
Cancer is an abnormal growth and proliferation of cell. Breast cancer is now the most common cancer in most cities in India and 2nd most common in rural India. The incidence of breast cancer is increasing in younger women. Because of lack of awareness and lack of screening it goes unnoticed till it becomes symptomatic. To create awareness about breast cancer is very essential.
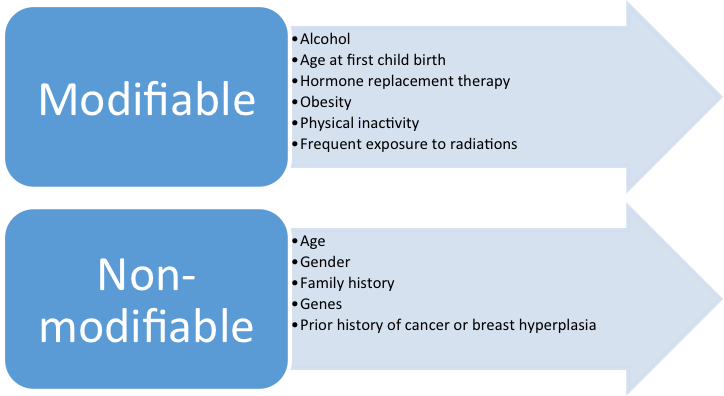
Breast cancer is caused by lots of different factors many of them are beyond our control. Broadly speaking the risk factors can be divided into modifiable and non- modifiable.
Breast cancer preventive strategies:
- Keep your weight in check
- Be physically active- 30 to 60 minutes of moderate intensity exercises which should be combination of strength, stamina and flexibility. 3-5 days/week
- Eat fruits and vegetables- Avoid too much alcohol
- Don’t smoke
- Breastfeed for 1 year after child birth if possible
- Avoid birth control pills especially after the age of 35 years
- Avoid post- menopausal hormones
- Know about family history
- Don’t forget screening.
Please seek a medical help if you have:
- A lump or thickening in the breast
- Redness, or soreness of skin
- Swelling and dimpling of skin
- Change in shape or appearance of the nipple-
- Nipple discharge
There are different types of treatment options for breast cancer survivals such as breast conservation surgeries, radiotherapy, chemotherapy, hormonal therapy and rehabilitation.
Physiotherapy plays an important role in rehabilitation of breast cancer survivals
Most of the women suffering from breast cancers has to go for complete breast removal or breast conservation surgeries and obviously post-surgery they have to undergo chemotherapy and radiation therapy.
As major portion of breast tissues, lymph nodes, nerves and muscles around the breast, shoulder and neck region are cut or spared depending upon the extent of cancer pain and swelling in the region of neck, shoulder and chest wall is very common. Also weakness of muscles around the shoulder region leads to stiffness and inability to do overhead activities. Postural impairments and Chemotherapy and radiotherapy related fatigue is also very common. Combination of these factors along with psychological trauma and stress leads to poor quality of life and lack of feeling of well-being.
Cancer rehabilitation:
It is a process to improve the physical and social function of the person suffering from cancer in order to improve quality of life and leading to longer survival.
Post operatively the physiotherapy aims at reduction of swelling by positioning of arm and elevation, gradual activities of wrist and hand, gradual mobilisation of shoulder and neck to prevent stiffness and to improve function. Gradual strengthening of muscles around shoulder and neck. Improving stamina through gradual planned exercise program.
Lymphadenopathy edema is the common complication after breast cancer surgeries. It can be prevented by following measures:
- Manual lymphatic drainage (form of a light massage in particular direction to drain the lymphatic fluid in proper channels)
- Multilayer elastic compression bandage or pneumatic compression
- Skin care- keep skin clean, hydrated. Use of gloves during household work.
- Regular exercise
- Weight control
Psychological support from families, friends and health care professionals is very essential to the women suffering from breast cancers.
Giving up is not an option, Believe there is a hope for a cure!!
- Dr. Aditi Kate
Screening for Sport
A fourteen year old boy who lives in America, but was vacationing in Mumbai came to me a few days ago. Let us call him Raj (name changed).
A footballer at the inter-school level, he was playing the sport for the last eight years.
Raj came with a history of an injury during a game that he played a month ago for his school. He was seen by the therapist from his team, but was now in my clinic because his parents were worried about an abnormal swelling that they saw in front of the knee.
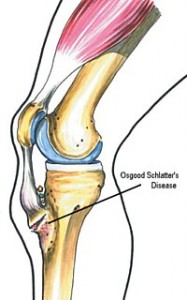
Actually what Raj had was a very common “Growing-Up” injury, which happens mostly in active adolescent boys. It is called Osgood Schlatter disease.
Muscles are attached to bones by strong bands (tendons), and as the muscle contracts strongly, the tendon pulls on the bone resulting in a movement at the joint. When a big growth spurt takes place (increase in height), sometimes bones grow faster than the muscles. While the length of the muscle is trying to catch up with the length of the bone, the shorter muscle ends up exerting a greater force than the tendon attachment can bear.
The Quadriceps is a four headed large and strong muscle in the front of the thigh and is attached by a relatively small tendon just below the front of the knee. In active adolescent children (Boys more than girls), this tendon sometimes pulls too hard on its attachment and dislodges a part of the bone there, causing pain, swelling, and a visible “bump” in front of the knee.
If given adequate rest and treatment, the pain and swelling usually resolves itself (The bump sometimes stays on, but it is not significant in sporting performance later). What usually happens though is that in severe cases (like this boy who came to me) a year or two of their sporting career is lost due to pain and enforced rest.
Can this be prevented? Maybe not. The small repetitive injuries that the strong pull of the muscle is causing cannot be detected early enough, and more often than not it is diagnosed only when significant damage has already occurred.
But here is what I feel very strongly about. Should children in sport not be regularly screened for growth spurts, tight muscles (something as important as the Quadriceps), and many other factors that commonly contribute to injuries? Should their exercise plans not be based on such findings?
The case in point (Raj) had such short Quadriceps that when he lay on his stomach, his knees could only bend to 90 degrees, whereas normally the heel should almost touch the buttocks.
He was with the team for eight years, he was a valuable member of the team, and was in their care during his growth spurt. Nobody noticed that he had such tight Quadriceps.
I do not know for certain and cannot prove that a good screening and concentrated stretching plan could have prevented his injury. But I do believe that perhaps it could have been prevented or at least its severity lessened.
This is not an isolated case, most children in sport are not screened with care often enough to predict and prevent injuries. Most children in sport are not important enough to get much individual attention, and almost none get individualised prehab exercises.
The sad consequence is that we lose valuable sporting talent, because the age that these injuries occur at is also the most crucial stage in their professional life: many talented children, if not adequately backed by parents and support groups, eventually give up on their chosen sport and pick another career.
Person! Not Diagnosis
A patient walked in to my clinic today (I had seen him a few years earlier) wondering if we could help him with his unique problem. He had just one complaint – For the last two years his handwriting had been deteriorating.
He is an intelligent, well-read, and knowledgeable individual of middle age, and he had already visited a few Doctors (including a Neurologist), got several blood tests done, and no one had found anything really wrong with him. He had been prescribed all the vitamins that could be required for a “nerve” problem, and he was diligently consuming them. He was active (in his own words, he would jog every day, but his speed had reduced over the last few years), worked at his job, and was in general healthy and well.
But he was frustrated – no one had a diagnosis, and no one had a solution. Meanwhile, his deteriorating handwriting made it difficult for him to sign, creating a practical difficulty. Besides, he was worried about it.
During a detailed examination, I found a slight weakness on the right side of his body, and a very slight imperceptible tremor. An intelligent man, he knew this himself and asked me if it could be Parkinson’s disease. Well it could be. But a Neurologist had done a detailed examination a few days ago, and had not diagnosed him.
So this is what I think: If we do not have a diagnosis, do we NOT treat the symptoms using simple non-threatening methods? Oh we take a Combiflam if we have a head ache for God’s sake! And this is a man complaining of a very specific weakness that is causing him problems for the last two years!
I will put him on a very specific exercise plan. We will start with strengthening of his Shoulder girdle muscles (Proximal stabilizers), and upper arm muscles. Over the next few weeks we will choose elbow and wrist muscles for our strengthening program, while increasing the work of the stabilizers. Lastly we will concentrate on fine motor skills, working on finger grip strength and functional tasks. In fact while we are at it, we may design a whole body routine improving flexibility, core strength, and lower body strength too, with his permission.
I cannot say with surety if my plan for him will work, but what’s the harm in trying? Besides, a well-planned strength training program rarely fails us. I am hoping to see him do better in the next few months: I will keep you posted!
The “How to use Manual”
I wrote this in 2010, but felt it was important to share it in my blog:
The “How to use Manual”
The human body is the only machine that does not come with a “How to Use” Manual. It is strange that such a complicated, well designed and priceless piece of engineering comes with no suggestions on maintenance and tips to use it better.. (Even my simple Nokia phone sends me daily tips on how to make the best use of it!!)
Most of us stumble through life learning about our bodies from other people’s experiences; or learning by ourselves as and when we need to: from friends, peers, elders, doctors, teachers, books, trainers, the internet, etc… Unfortunately, all the people we learn from are themselves clueless or half informed because you see, there are no tips from the manufacturer himself!! In fact, since the manufacturer was a designer, he has made each of us unique, and actually there is no human exactly like another.. (Proven by the fact that each of us has a fingerprint that is unique). This means that any amount of research done on the human body cannot be absolute, and cannot be precisely applied to all humans unfailingly. Why then are we so smug about our knowledge of our bodies, why do we not hesitate ever so slightly when advising others based on what worked for us, or what we studied to be correct? When in fact, the only thing we are sure of is that we cannot be sure of anything!
Our concepts of “hygiene” and “looking after the body” are largely dependent on our geographical location, culture, financial position, gender and generation. They also depend up on the personal beliefs of the people raising us: Parents, Relatives, Guardians, and such.. So for example whether to brush your teeth once a day, twice or thrice in a day, or whether to brush your teeth at all, may depend on your cultural and social background or upbringing. Some of these also depend up on professional requirements and financial constraints. E.g. an actress may spend several thousand rupees on beauty treatments per month, and a housewife may spend a few hundreds. In fact if we think about it none of these so-called “looking after your body” concepts are a part of normal human development. These are cultural and social “learnt” concepts, and though a necessary part of living in today’s world, not natural or necessary to the human body.
What is most natural to the human body, and an essential part of development (as in all animals) is “Movement”. We do not need to be taught how to “move”; a foetus starts moving in the mother’s womb at the age of seven weeks and continues to learn “motor skills” throughout infancy and early childhood. Anyone that has seen the joy on a child’s face as he takes his first step, or the exhilaration that a child feels as he runs freely in a field, cannot doubt that this is what the human body was designed for.
Social and cultural rules and norms actually rob us of our right to free movement around the time that we enter full time school at the age of six (think about the teacher insisting the child sits still in a chair for hours aiming for cerebral growth, but slowly un-learning motor skills), and by the time we are done with formal education somewhere in our twenties, we have forgotten the joys of free movement. Exercise now becomes a chore, one more thing to be “fitted” into our “to do” list for the day. Some of us may even ignore this most essential “Looking after our body” routine till health fails. We now need help to learn afresh “How to move”! This help comes from fellow humans, who have learnt these skills from other “Older, more experienced” humans and have probably been certified by institutions and academies run by “Even older and even more experienced” ….HUMANS!!
The human body is a marvel of engineering: so uniquely designed with so many components working together tirelessly through life in the best example of teamwork. It is also an ever-changing and evolving piece of art and each individual is different from one day to the next. Each of us is unique, and none other in the world is exactly the same. It is not possible to completely understand the human body in a way that we can apply our knowledge unerringly to all that we try to help; thinking that we can, in fact is grossly arrogant and audacious. All of us in the field of medicine know that one of the first things we learn in Medicine is “Differential Diagnosis”. We arrive at a diagnosis not with conviction but by elimination, and hence it is our duty to remain “slightly uncertain” in the interest of the patient. It will also help to remember that no research ever gives a 100% conclusion, and all our treatments are based on what works for a “larger” percentage of the population.
All of us in professions dealing with the human body (Doctors, Trainers, Coaches, etc.) need to tread lightly, cautiously and with humility because we do not have that “How to use” manual.
Tennis elbow and a series of unfortunate accidents
What is “Tennis Elbow” and why does it take so long to heal? Is it because it is an incurable/ poorly understood condition or do a series of unfortunate events lead to its delayed healing?
First of all, though it is called Tennis Elbow, it rarely affects those that play tennis regularly. To put this precisely, Tennis elbow is usually caused by ‘overexertion’, usually in some ‘unaccustomed’ activity.. It can be either somebody trying to perfect a weak stroke by repeatedly striking the ball in a new style, or a regular cyclist playing an extended game of tennis all of a sudden, or a recreational athlete playing a tennis tournament requiring him to play tennis everyday (something that he was unaccustomed to): a tennis player practising/ playing every day in his natural style rarely suffers a “Tennis Elbow”.
Tennis elbow can of course happen without holding a tennis racquet at all.. eg. If an upper body workout was suddenly increased in intensity, or some heavy furniture was handled during renovation, a cricketer changes his bat, chooses a slightly heavier one and does an extended practice session with it, etc. The pain usually starts after an elongated period of repetitive, strenuous, unaccustomed movement. Though the patient is not usually aware at this stage that he has tennis elbow, we will call this “Stage 1”
The pain usually starts as a minor niggle that can be easily ignored. It is usually a slight discomfort or dull ache on the outside of the elbow, the upper forearm. The pain may be transient, and not dramatic enough to seek help. Since the pain has come on due to an activity that the person has chosen to do (not really a one-time activity), the person is more often than not going to repeat that activity for a few days/ weeks: for e.g. If a cricketer has bought a new bat he is going to continue practising with it; If a tennis player is perfecting a stroke, he is going to continue practising it; If a tournament is going on, the player is going to play matches everyday; If a house is being renovated, the person may shift things around every day. The pain becomes worse because the same repetitive, strenuous, unaccustomed movement is repeated daily for days or weeks till the onset of acute pain. This is usually when the patient seeks help, and we will call this “Stage 2”
The healing response in the human body is very strong and at “Stage 1” itself, the cells surrounding the site of tendon injury are activated to mobilize repair material to reconstruct the damaged tendon. This involves excess blood, disruption of some tissue and increase in the number of new cells, all of which increase the “Swelling” or “inflammation” in that area. A few days of rest from the aggravating strenuous activity taken at this stage, will let the body heal itself. Unfortunately, we do not always listen to the small signals our body gives us, and this healing reaction is wasted by repeating the stressful activity and leading to “Stage 2”.
In “stage 2”, the body’s healing mechanism is still trying to repair the damage, but due to a larger area of damage, more disruption of tissue and larger collection of blood, now the healing process works against the tendon, and immature, dysfunctional cells are generated.
Because the patient has now asked for help, help comes from all directions. He will be asked to take rest for a week or two, also given physiotherapy, medications, massage, compressive brace, etc. More often than not, none work immediately at this stage, and the patient is not much better after 1 week. We must remember that it is very difficult to “give rest” to the wrist extensors at this stage because they are involved in all hand functions! In fact even lifting a teacup or a sheaf of papers is difficult and painful!
Two to three frustrating weeks have now passed and if the patient is a sportsman, he is not ready to wait any longer. He is probably training for a major tournament (he was perfecting a stroke when he got injured) or is insecure about his place in the team, or just does not like being away from his sport. His friends are advising him to try something different, his colleagues are practising hard, his family is worried, and he is unhappy and edgy.
He revisits his surgeon, or goes to another, and seeing that he is so impatient, they now suggest “PRP” or “Steroid injection” for pain relief.
“PRP” or platelet-rich plasma is increasingly being used for tissue healing of all kinds. Blood harvested from the same person is processed to make the PRP and is injected at the site to enhance healing. It has been proved that it releases at least 7 different growth factors that stimulate healing in bone and tissues.
“Cortisone” is a natural steroid that is made by our body in adrenal glands, and released in times of stress. The injectable cortisone is synthetically made, but has the same composition as the natural one, and is used for local injection (In to site of pain). It reduces pain by reducing inflammation (swelling) and has no role in tissue healing. In fact by its very effect (reducing inflammation), it PREVENTS tissue healing.
Let us examine the effect of either of these two choices. Though the trend is changing, the steroid shot is usually (unfortunately) tried BEFORE the PRP.
The “Steroid shot” is given so that the player can resume play. The steroid injection can bring about pain relief after 2-3 days and if it works, the effect can last for several months or years. Unfortunately, sometimes it does not work, or sometimes also increases pain tremendously due to “crystallization”. If it does work, remember it has not caused any healing, only pain relief and compromised the healing process. If pain relief occurs, the player is going to resume play within a week, and increase intensity immediately to make up for lost time. He will also probably wear a compressive brace to protect the tendon.
If the player is young and has injured his elbow for the first time without too much damage, he may not get a recurrence of symptoms. If, on the other hand he is older, and has had a worse damage, the case will be completely different.
Tendons have a lower blood supply than muscle fibres. The function and structure of muscle and tendon is different, but they are both contractile in nature, and both need energy to work (contract). Tenocytes (Tendon cells) produce their own energy by aerobic and non-aerobic processes going on inside them. “Aerobic” processes require oxygen, which is carried to the cell by blood, and obviously, when blood supply is lower, the aerobic capacity decreases. But aerobic energy generation is the most profitable and desired by the cells. In sporting activities that go on for long hours at a time, eg. Tennis, Batting, etc. aerobic energy production is very important. In older tendons, blood supply is further reduced, and is actually 7 times less than younger tendons!! Obviously then, in an older athlete, with an injured tendon, especially after the steroid shot when blood supply is suppressed, the aerobic energy generation of the tendon is compromised. This is actually made worse by the compressive “Tennis elbow support” that he is wearing. Without sufficient aerobic energy, the tendon is forced to use the less efficient anaerobic systems, which lead to a build up of toxic material causing pain and inflammation to increase.
It is now 5 weeks since the player first noticed pain, and he is again in pain and discomfort, very unsure of whether to continue playing or to take rest again. He meets his surgeon, and again the surgeon has two choices: 1. Repeat the Steroid shot, and 2. Try PRP now.
More often than not, Steroid will be given one more chance. The whole process is now repeated again, but the steroid now may have weakened the tendon and cartilage (one of the known side effects of steroids). Now when the player plays or trains, he is at risk of actually damaging/ tearing the weakened tendon more!! Once again, pain may or may not subside, but the tendon is now more at risk, and at least 8 frustrating weeks have gone by!
If, on the other hand, the surgeon chose PRP before the first Steroid shot (3-4 weeks after first pain was noticed), let us examine what might happen.
As opposite of Steroid shot, PRP is given so that the tendon might heal. The surgeon here is assisting the body’s own healing mechanism by introducing platelets that will promote healing. Unfortunately as this technique and assumption is not fully understood as yet, and not too many studies (clinical trials) have been conducted, the surgeon and the patient may have different expected outcomes. Though the surgeon is giving “healing” a chance, the player probably thinks he will get quick pain relief. Ideally after PRP, a week of rest and light stretching, followed by light activities and gentle strengthening for 2 weeks, and then a gradual (over 2-3 weeks) return to play/ normal activities is advocated. This gives time for the healing process to be completed (tendon repair by the body takes between 6-10 weeks to complete). The player’s haste to play, and the surgeon’s need to prove the efficacy of the technique may end up compromising the healing process by the decision to resume training/ play early (usually the player tries to start training in a week after the shot, and resumes play within 2-3 weeks). If luck and age is on his side, all might go well and he will be rid of the symptoms. But more often than not, this haste is detrimental, and then another shot of PRP or now of Steroid is tried.
If PRP was not tried at 4th or 5th week, and the player has taken 2 shots of steroid, PRP has almost no chance of working after 8-10 weeks. By now the tendon is weakened, damaged beyond repair, has extensive connective tissue damage, and is in a chronic inflammatory stage (here the inflammation is not curative, but more “degenerative” in nature). The principles of treatment that apply to inflammatory conditions cannot be applied here. In fact once in the degenerative stage (Tendinosis), all treatments work by “trial and error”.
When in a chronic stage, all treatment in tennis elbow is palliative. Pain relief using drugs, electrical stimulation, heat, ice, massage/ manual techniques should be achieved along with a planned “Tensile loading” using all the principles of exercise science. Gradual strengthening, eccentric training, flexibility exercises to prevent adhesions, and “activity specific” training, all help if care is taken not to damage the tendon further. Taping and bracing for short periods of time help, if used with care. It is important to understand that what works for one patient may not work for another, and a short daily assessment is required.
If all else fails, after several months, the surgeon may advise a surgery to relieve the symptoms. This is of course an invasive procedure, and during surgery, either the tendon sheath is trimmed, or the tendon itself is released from the bone. In most patients, surgery gives the required pain relief after 3-4 weeks, and return to normal activities in 4-6 weeks is expected. Return to play takes 12-16 weeks, a full 12 months after the patient first felt a twinge of pain!!
Though Tennis elbow is known as “Lateral epicondylitis”, the physiology of exact damage is not understood. Tendonitis, tendinosis, tenosynovitis, peri-tendonitis, etc. are the several names given to injuries/ conditions affecting the “muscle-tendon” unit. The exact nature and area of injury cannot be determined by an examination and even after using various diagnostic tools available (Imaging: US, MRI) we will only be slightly better informed. Though some research is available on the acute inflammatory stage of tendon damage, a major drawback to understanding the chronic tendinopathy is that there are no suitable animal models available for research on chronic tendinopathies! Obviously, animals take rest when injured and let their body heal naturally. The only animal models available for research are Race Horses, who suffer similar chronic tendinopathies as humans! They are obviously not suitable subjects for research, and now research is going on by artificially creating such injuries on rabbits.
The natural process of tendon healing after an acute onset takes about 9-10 weeks to complete and goes through the inflammatory, proliferative and remodelling/ consolidation phases. Restricting activity in the first 2-3 weeks after injury, using available treatments at that stage to help healing without causing further damage, then introducing a flexibility and light strengthening program in the second or third week, increasing the loads and adding eccentric strengthening in the fourth to sixth week and introducing sport-specific strengthening from the 7th to 9th week will ensure that the return to play is smooth and incident-free. All treatment options available do have a role to play at different stages of healing, but should be applied after evaluating their efficacy at the stage, and the goals and expectations of the player/ patient. For eg. If the player has a major international tournament of great significance to his career, suppressing the inflammatory process with a local steroid shot is warranted and acceptable. Of course explaining the expected outcome to the player is crucial. But if there is no urgent need for intervention, it is best to play a supportive role to nature and use simple modalities like therapeutic US, electrical stimulation and a wise use of exercise and taping to assist the healing process.
Understanding the physiological and pathological processes going on in the body and conveying the need to “Go slow” effectively to the patient is the duty of the advising Doctor/ professional. Players are often overwhelmed by the diversity of advice and treatment options available, are under various pressures of their own, and their team members and coaches probably have expectations which they need to fulfil.
Tennis elbow then is not poorly understood, nor incurable, but is a series of unfortunate events/ decisions/ actions/ accidents often leading to a very long period of pain and stress!